8 reasons why your cough is not improving!
Coughing is a protective reflex of the body and helps clear particles and secretions from the lungs. However, sometimes a cough can become a chronic condition.
A chronic cough is usually defined as a cough that lasts for eight weeks or longer. Continuous coughing can be annoying and embarrassing. It can make you physically tired, disturb sleep, and may cause dizziness, hoarseness, muscle strain, sweating, and urinary leakage (especially in women).
If your cough is not improving for a long time or keeps recurring frequently, you may have one of the following medical problems:

Common Causes of Chronic Cough
1. Postnasal Drip
Postnasal drip occurs when secretions from the nose flow into the back of the throat. These secretions can irritate the throat and trigger a cough. It commonly occurs in people with allergies, colds, rhinitis, and sinusitis.
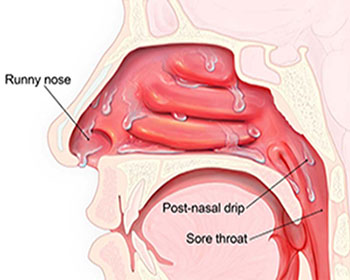
Symptoms include a stuffy or runny nose, a sensation of liquid in the back of the throat, and frequent throat clearing. Some individuals have “silent” postnasal drip, where cough is the only symptom.
2. Asthma
Asthma is the second most frequent cause of chronic cough in adults and the leading cause in children. In addition to coughing, patients may experience wheezing or shortness of breath.
In cough variant asthma, cough may be the only symptom. Asthma-related cough may be seasonal, follow an upper respiratory infection, or worsen with exposure to cold air, dry air, fumes, or fragrances.

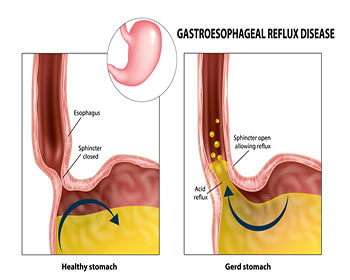
3. Acid Reflux (GERD)
Gastroesophageal reflux occurs when acid from the stomach flows back into the esophagus. GERD refers to symptoms caused by this reflux.
Many patients experience heartburn or a sour taste in the mouth, but in some individuals, cough may be the only symptom of GERD.
Other Causes
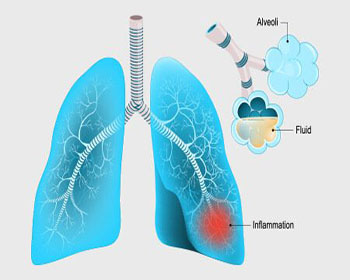
4. Respiratory Tract Infection
Upper respiratory infections such as the common cold can cause cough lasting more than eight weeks. This may be due to postnasal drip or airway irritation following infection.
Bacterial tracheobronchitis or bacterial sinusitis may develop after a viral infection. These conditions often cause a productive cough with sputum that may be yellow, green, or brown.
5. Use of ACE Inhibitors
Angiotensin converting enzyme (ACE) inhibitors, commonly used to treat high blood pressure, can cause chronic dry cough in up to 20 percent of patients.
Switching to an alternative medication usually improves symptoms within one to two weeks.
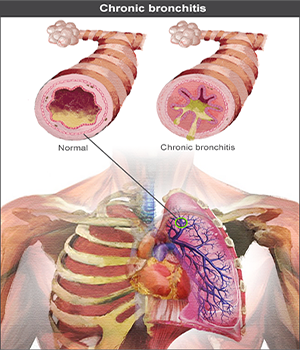
6. Chronic Bronchitis
Chronic bronchitis causes airway irritation leading to persistent cough, often with phlegm production. Most affected individuals are current or former smokers.
7. Lung Cancer
Lung cancer can cause coughing, though it is a rare cause of chronic cough. It should be suspected particularly in smokers if the cough changes suddenly, blood is coughed up, or the cough persists beyond one month after quitting smoking.
8. Eosinophilic Bronchitis
Eosinophilic bronchitis is a less common cause of chronic cough and involves airway inflammation without features of asthma.
Breathing tests are normal, but sputum or airway biopsy shows increased eosinophils.

Diagnosis of Chronic Cough
To determine the cause of a chronic cough, your healthcare provider will review your symptoms and perform a physical examination.
Based on clinical findings, a trial of treatment may be recommended before further testing. If symptoms improve, no additional tests may be needed. If symptoms persist or diagnosis remains unclear, further evaluation may include:
- Lung imaging: Chest X-ray or CT scan, especially in smokers or patients with lung-related conditions
- Lung function tests: Performed when asthma is suspected but not confirmed clinically
- Acid reflux testing: Esophageal pH monitoring or upper endoscopy to evaluate GERD
Dr. Sagar Raiya's Publications
See Our all publications and presentations
